This site is supported by our readers. We may earn a commission, at no cost to you, if you purchase through links.
A single millimeter can determine whether an injection delivers relief or triggers complications that persist for months. When healthcare providers select needles for administrations, they must account for patient anatomy, medication viscosity, and the precise tissue layer requiring drug deposition—yet selection errors occur more frequently than most patients realize.
The consequences of using incorrect needle gauge or length extend far beyond momentary discomfort at the injection site, affecting everything from medication absorption rates to the formation of nerve damage and chronic inflammatory responses.
Understanding what happens if you use wrong needle specifications illuminates why medical protocols emphasize rigorous verification procedures and why seemingly minor equipment decisions carry significant clinical weight for patient outcomes and long-term tissue health.
Table Of Contents
- Key Takeaways
- What Happens if You Use The Wrong Needle?
- Common Problems Caused by Incorrect Needles
- How Wrong Needle Size Increases Infection Risk
- Effects on Medication Effectiveness
- Long-Term Complications of Needle Errors
- Preventing Needle Selection Mistakes
- What to Do After Using The Wrong Needle
- Frequently Asked Questions (FAQs)
- Conclusion
Key Takeaways
- Using the wrong needle gauge or length can cause immediate tissue trauma, nerve damage, and hematoma formation, while also compromising medication absorption by depositing drugs in unintended tissue layers that alter therapeutic effectiveness.
- Incorrect needle size increases infection risk through larger puncture wounds that expose more surface area to pathogens, and may cause long-term complications including chronic pain, numbness, scar tissue formation, and reduced mobility that persist for months or years.
- Healthcare facilities can prevent needle selection errors by implementing systematic verification protocols, requiring dual staff confirmation of needle specifications against patient requirements, and maintaining rigorous training programs focused on proper needle calibration.
- If you’ve used the wrong needle, you should immediately assess the injection site for bleeding, swelling, or unusual pain within 15 minutes, contact your healthcare provider for persistent symptoms or signs of nerve damage, and monitor for complications during the critical first 24 hours.
What Happens if You Use The Wrong Needle?
Using the wrong needle during an injection can trigger a cascade of complications that affect both immediate outcomes and medication effectiveness. The consequences range from visible physical reactions at the injection site to less obvious problems with how your body absorbs the medication.
Understanding these three key areas will help you recognize why proper needle selection matters so much for patient safety and treatment success.
Our comprehensive knitting needles buyer’s guide walks you through materials, sizes, and styles so you can match the right needle to every project.
Immediate Physical Effects
The moment a needle of the wrong gauge pierces your skin, a cascade of unintended physiological responses begins—ranging from heightened pain sensation to localized tissue disruption that extends far beyond the intended injection site. Understanding proper needle gauge sizes is essential to minimize these risks.
An oversized needle creates excessive physical trauma, tearing through dermal layers and causing immediate tissue damage that manifests as sharp, stabbing discomfort. Conversely, needles that are too small require increased insertion force, intensifying pain management challenges and potentially leading to nerve injury or injection complications at the site.
Understanding how to troubleshoot common industrial sewing issues helps prevent these needle-related complications before they compromise fabric integrity or operator safety.
Both oversized needles and needles that are too small cause excessive tissue trauma, intensifying pain and risking nerve injury at the injection site
Impact on Medication Delivery
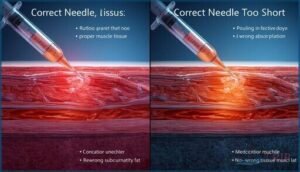
Beyond the immediate discomfort of using an incorrect needle size, your medication delivery can be compromised in ways that directly affect treatment outcomes. Wrong needle gauge or length alters injection depth, influencing how quickly the medication enters systemic circulation and achieves therapeutic bioavailability.
Choosing the right needle isn’t just about comfort—understanding needle specifications ensures your injection delivers medication at the intended depth for optimal absorption.
- Viscous solutions may be incompletely delivered, reducing medication absorption and necessitating dose adjustment
- Incorrect needle length deposits drugs in wrong tissue layers, altering the intended injection depth
- Too-short needles in intramuscular injections cause subcutaneous administration, delaying onset of action
- Mismatched needle size can require re-administration to achieve proper medication delivery
- Tissue layer mismatch fundamentally disrupts the pharmacokinetics of your medication administration
Patient Comfort and Pain
Patient comfort during needle-based procedures depends heavily on proper needle size selection. Incorrect gauges cause measurably higher pain scores and anxiety levels.
Sewing enthusiasts face similar challenges, where choosing the right sewing machine needle prevents fabric damage and thread breaks.
When you use a needle that’s too large, you’ll experience more tissue trauma and nerve damage risk. Overly small gauges require excessive insertion force, increasing procedural pain and extending discomfort duration beyond the typical 1–5 minute post-injection window.
Common Problems Caused by Incorrect Needles
When you use the wrong needle, the consequences extend beyond momentary discomfort and can lead to serious physical complications that affect both immediate and long-term patient outcomes.
These problems often stem from mismatches between needle gauge, length, and the specific requirements of the injection site or medication being administered.
The most frequently observed complications include tissue trauma with associated bruising, damage to peripheral nerves, and the formation of hematomas at the injection site.
Tissue Trauma and Bruising
When you use the wrong needle gauge, your injection can rupture small blood vessels, causing bruising that shifts from red-to-purple to brown over several days. Tissue trauma from incorrect needle selection creates localized swelling and tenderness that generally persists for 24–72 hours, while deeper injections through fragile tissue increase your risk of hematoma formation.
Choosing the right needle diameter and length—guided by detailed needle size guidelines—minimizes vascular damage and reduces post-injection complications.
- Repeated injections in the same area cause cumulative vascular disruption and microtrauma
- Anticoagulant therapy and clotting disorders markedly heighten your bruising risk
- Proper injection techniques minimize tissue damage and support faster wound healing
Nerve Damage Risks
Direct needle contact with peripheral nerves produces immediate sharp pain and radiating paresthesias, signaling potential injury during injection. The risk profile varies by anatomical site, with axillary and sciatic regions carrying elevated vulnerability due to their proximity to major neural structures. Incorrect needle gauge or aggressive insertion techniques can compound nerve trauma and neurological effects.
| Injury Type | Onset & Symptoms | Recovery Timeline |
|---|---|---|
| Neurapraxia | Immediate numbness, tingling | Days to weeks |
| Axonotmesis | Motor weakness, sensory loss | Months, may require therapy |
| Direct transection | Severe pain, complete deficit | Variable, often permanent |
Electromyography and nerve conduction studies help distinguish injury severity, guiding pain management and determining whether referral to a neurologist is warranted when deficits persist beyond expected recovery windows.
Hematoma Formation
Hematoma formation occurs when your needle punctures a blood vessel during injection or phlebotomy, allowing blood to pool in surrounding tissues. Incorrect needle gauge—especially larger diameters—intensifies tissue trauma and vessel injury, disrupting normal hemostasis and delaying vessel repair.
You’ll notice swelling, tenderness, and discoloration within hours as the hematoma expands, particularly if you’re on anticoagulants or have clotting disorders.
How Wrong Needle Size Increases Infection Risk
Infection risk increases markedly when you use the wrong needle size, creating vulnerabilities that allow pathogens to enter your body.
The size of the puncture wound and the sterility of the equipment both play critical roles in determining whether bacteria can establish an infection at the injection site.
Understanding these two key factors will help you recognize why proper needle selection is essential for infection prevention.
Larger Puncture Wounds and Bacterial Entry
When you use a needle gauge that’s too large, the resulting puncture wound exposes a greater surface area to skin flora and environmental pathogens, directly increasing bacterial entry and infection risk. Deeper tissue damage disrupts multiple tissue planes, creating spaces where bacteria evade your immune defenses.
Clinical guidelines consistently link larger needle size to higher infection rates and delayed wound healing, making proper needle gauge selection a critical infection control measure.
Improper Sterilization Consequences
Sterilization failure creates contamination pathways that compromise infection control protocols, allowing microbial transmission through reused or inadequately processed equipment and increasing healthcare-associated infections.
Residual sterilant chemicals pose chemical exposure risks to tissues, while biofilm formation on improperly sterilized surfaces reduces disinfectant efficacy.
Device rejection from compromised sterilization delays necessary medical procedures, directly undermining patient safety measures designed to prevent infection risk.
Effects on Medication Effectiveness
When you use the wrong needle size, the medication itself may not work as intended, regardless of whether it’s the correct drug or dosage. The physical properties of the needle—its gauge and length—directly influence how the medication enters your body and how effectively it reaches the intended tissue.
Understanding these two critical factors can help you recognize why needle selection matters beyond just comfort or safety.
Incomplete or Delayed Drug Absorption
When absorption via the injection site slows, you may experience a delayed onset of action, extending the time to reach peak plasma concentration and compromising drug bioavailability. Improper injection depth can redirect medication into subcutaneous tissue rather than muscle, while viscous medication formulations face inherently slower absorption rates.
Local tissue conditions like edema further impair perfusion, introducing pharmacokinetic variability that may necessitate dose adjustments.
Impact of Needle Gauge and Length
Your needle’s gauge and length don’t just determine comfort—they control how accurately medication reaches target tissue. When you use the wrong size, you risk injection depth errors that redirect doses into unintended layers, compromising absorption and effectiveness.
- Larger gauge numbers require more force, potentially slowing medication flow
- Longer needles access deeper anatomical planes, improving intramuscular delivery precision
- Shorter needles increase subcutaneous dosing errors for deep injections
- Needle deflection and tissue shear create dose uniformity problems across repeated administrations
- Needle flexibility varies with gauge, affecting penetration accuracy and nerve damage risk
Long-Term Complications of Needle Errors
While most needle errors cause temporary discomfort, some complications don’t resolve quickly and can affect your health for months or even years.
The consequences extend beyond initial pain or bruising, creating ongoing challenges that interfere with daily function and quality of life. You should understand these potential long-term effects, which include persistent neurological symptoms and structural tissue changes.
Chronic Pain and Numbness
Nerve damage from improper needle gauge or injection techniques can trigger chronic pain that persists for months or even years, often presenting as dysesthesia or paresthesias that disrupt daily activities and sleep.
Chronic inflammation along affected nerve pathways may require specialized pain management and sensory rehabilitation, particularly when injections traverse neural-rich regions, making early intervention critical for neural recovery.
Scar Tissue and Reduced Mobility
Beyond lasting nerve pain, repeated tissue trauma from incorrect needle size can trigger scar formation and fibrosis that restrict movement over time. Chronic inflammation around injection sites reduces tissue elasticity, while muscle atrophy may develop when mobility issues prevent normal use of affected limbs.
Proper injection techniques and early fibrosis management through physical therapy help preserve function and minimize long-term tissue repair complications.
Preventing Needle Selection Mistakes
Needle selection errors are largely preventable when healthcare facilities implement systematic safeguards and maintain rigorous standards. You can greatly reduce the risk of complications by following established protocols for needle size determination, ensuring your staff receives thorough training, and instituting mandatory verification procedures before any injection.
The following sections outline three critical strategies that form the foundation of safe needle practices in clinical settings.
Guidelines for Choosing Needle Size
Selection of appropriate needle size for medical procedures such as injections and phlebotomy requires systematic patient assessment, considering age, weight, tissue depth, and body site. Institutional protocols guide injection depth and needle calibration decisions.
You must verify syringe compatibility with the chosen needle gauge and needle material to ensure secure fitting. Always implement a double-check process before administration to prevent errors and enhance patient outcomes.
Importance of Staff Training and Education
Even with clear clinical guidelines in place, staff competency relies on consistent professional development and training programs that reinforce injection safety principles.
Healthcare quality improves when education standards mandate ongoing certification in needle selection, reducing medical procedure complications and medical error prevention rates.
You benefit directly when your clinical team demonstrates mastery of patient safety protocols through structured, evidence-based curricula.
Double-Checking Equipment
Before every injection, your clinical team must implement a standardized Equipment Verification checklist that confirms needle type, gauge, and size match the physician’s order and patient requirements. This systematic Needle Inspection protocol requires two staff members to independently verify needle parameters against documentation, recording results with timestamps in both the patient chart and equipment log to guarantee Medical Device Safety and prevent medical errors.
- Visual and tactile inspection confirms packaging integrity, ensuring sterile barriers remain intact before needle use
- Dual verification by independent Staff Training-certified personnel catches discrepancies that single-person checks miss
- Pause-and-verify protocols stop procedures immediately when labeling becomes unreadable or parameters don’t match orders
- Documentation with timestamps creates an auditable trail that strengthens Patient Safety and accountability across Medical Protocols
- Integrating Injection Safety checklists into workflow transforms medical safety from abstract principle into concrete, repeatable action
What to Do After Using The Wrong Needle
If you realize you’ve used the wrong needle during or after an injection, quick action can minimize potential complications and guide appropriate next steps.
Your response should be methodical, focusing on immediate patient assessment, determining whether professional intervention is needed, and establishing a monitoring plan for any delayed effects.
The following steps outline a systematic approach to managing this situation safely and effectively.
Immediate Assessment Steps
You must inspect the injection site within 15 minutes for bleeding, swelling, or unusual pain—these signs can signal complications from needle gauge errors that compromise patient safety. Monitor for adverse reactions like dizziness or rash, assess circulation, and document all findings immediately. Double-check patient identity, medication, and dose to prevent compounding medical errors before notifying your supervising clinician.
| Assessment Priority | Timeframe | Key Indicators |
|---|---|---|
| Injection site inspection | Within 15 minutes | Bleeding, swelling, pain |
| Patient monitoring for adverse reactions | Within 30 minutes | Dizziness, itching, rash |
| Emergency response evaluation | Immediate | Airway, breathing, circulation status |
When to Contact a Healthcare Provider
You should contact your healthcare provider immediately if you notice persistent bleeding, rapidly increasing swelling, severe pain that doesn’t subside within an hour, or signs of infection such as redness, warmth, or discharge at the injection site.
It’s vital to understand the causes of post injection inflammation to take proper preventive measures. Healthcare providers can assess potential complications, including nerve damage, that may require urgent medical procedures to guarantee patient safety.
Emergency signs warranting immediate medical guidance include numbness, tingling, or loss of sensation radiating from the injection site, which necessitate follow-up care under established healthcare protocols to provide appropriate patient support and prevent long-term consequences.
Monitoring for Complications
After a needle error, vigilant Post Injection Care becomes your safest defense. Essential Sign Monitoring during the first 24 hours helps detect bleeding or shock, while Patient Observation for swelling, warmth, or discharge at the injection site signals potential complications.
Watch for nerve damage symptoms—numbness or tingling—and document any hematoma or tissue trauma. Complication Signs require prompt Adverse Event Reporting to prevent long-term consequences from escalating unnoticed.
Frequently Asked Questions (FAQs)
Can wrong needles affect vaccine immunity development?
Improper needle gauge or length can misdeliver vaccine into subcutaneous tissue instead of muscle, potentially reducing antigen uptake and altering immune response quality.
Though direct evidence linking needle calibration errors to long-term immunogenicity remains limited, such errors may impact vaccine efficacy.
Do needle errors increase liability for healthcare facilities?
When the chips are down, needle errors dramatically increase facility risk through malpractice claims and regulatory actions.
Medical negligence in medication administration elevates liability insurance costs while compromising patient safety for healthcare providers.
How does needle length affect intramuscular injection depth?
Intramuscular depth depends directly on needle length relative to subcutaneous tissue thickness. A 25 mm needle usually achieves proper muscle penetration in most adults, but inadequate length results in subcutaneous deposition, altering drug absorption and vascular exposure.
Are certain patient populations more vulnerable to errors?
As the saying goes, “the weakest link breaks first.” Elderly patients face heightened risks from fragile skin, while pediatric care demands precision with smaller needle gauges.
Disabled patients, those with obesity factors, and individuals managing chronic conditions accumulate greater exposure to injection safety complications, nerve damage, and compromised patient experience.
What role does needle bevel orientation play?
The bevel’s angle and direction greatly affect insertion resistance, tissue trauma, and injection technique success. When positioned correctly—usually up for most subcutaneous and intravenous injections—you’ll reduce patient discomfort and vascular complications.
Conclusion
The next injection you receive may depend on decisions made in seconds—selections that separate uneventful procedures from complications requiring months of intervention.
When healthcare providers understand what happens if you use wrong needle specifications, they transform routine administrations into precisely calibrated interventions that respect tissue integrity and enhance therapeutic outcomes.
Every verification step, every gauge confirmation, and every length measurement represents your protection against preventable harm that begins with a single, irreversible puncture.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2769648/
- https://www.myvaccinelawyer.com/vaccine-injury-lawyer/resources/incorrect-intramuscular-injection
- https://diabetesonthenet.com/journal-diabetes-nursing/consequences-of-using-inappropriate-insulin-syringe-needle-lengths/
- https://www.nysora.com/education-news/mastering-iv-catheter-gauge-selection/
- https://dopinglinkki.fi/en/info-bank/other-information/risks-of-intramuscular-injection/